Medically Reviewed by: Yasir Ahmed, M.D.
When is a Corneal Transplant Necessary?
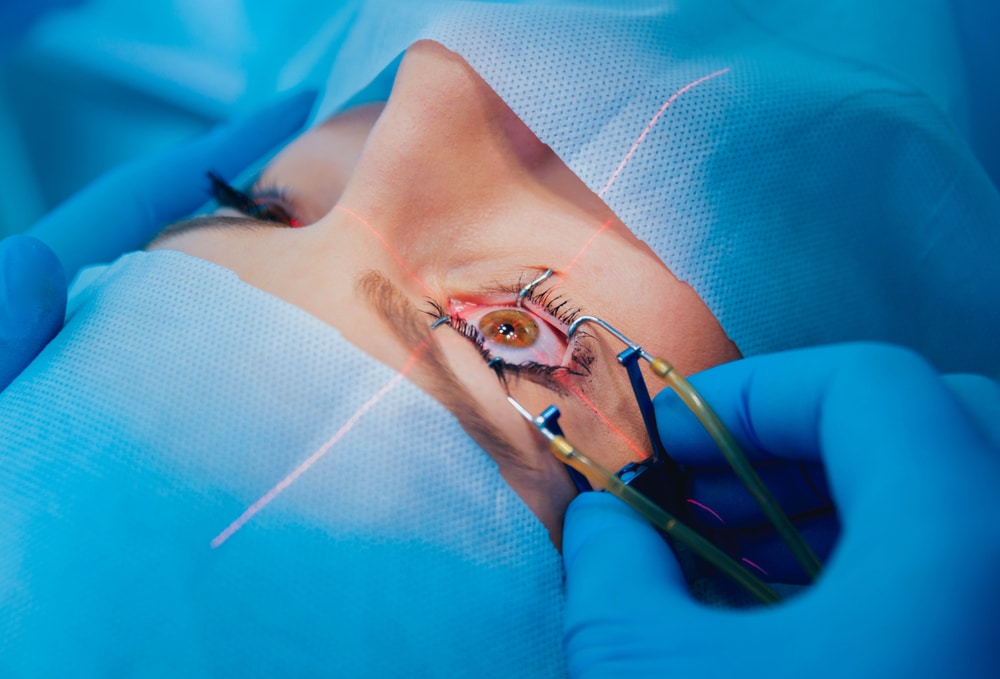
Damage to your cornea can negatively affect your vision as well as cause pain and irritation, and while surgery is not always the first line of defense, it can be a useful tool to relieve pain and restore your vision –– but exactly when is a corneal transplant necessary?
Cornea damage negatively affects your eyes’ ability to filter and focus light, resulting in blurred vision and intense glare. There are many reasons why your cornea could be damaged, ranging all the way from a simple infection to a degenerative condition, some of which can be treated with things like antibiotics or corrective eyewear. Corneal transplants are often necessary when glasses or contact lenses cannot restore your vision fully, or if infected tissue needs to be removed.
What is a corneal transplant?
A corneal transplant is the surgical removal and replacement of the damaged cornea with new, donated tissue. There are a few types of corneal transplantation:
- Penetrating keratoplasty: Also known as full-thickness corneal transplant, replaces all the layers of tissue of your cornea (usually in a small area). This is often performed to treat severe cornea damage.
- Lamellar keratoplasty: Also known as partial thickness corneal transplant, involves the replacement of only the outer and middle layers of your cornea. This less invasive procedure offers a speedier recovery and is often recommended for those who do not have severe damage or scarring.
- Endothelial keratoplasty: An inner layer corneal transplant, is usually only recommended to combat Fuchs’ dystrophy and other rarer medical conditions; this involves the replacement of only the innermost layer of your cornea.
Your ophthalmologist will recommend which surgery is right for you based on your specific needs. The surgery itself is an outpatient procedure that generally takes under two hours.
Top reasons why a cornea transplant may be needed
So, what conditions require corneal transplant? Not all corneal problems indicate a need for surgical intervention, but these conditions could indicate the need for a transplant:
- Scarring left behind by infection: people who wear contact lenses are at a higher risk for infection because of both the need for constant lens cleaning and changing and the increased physical contact with the cornea.
- Keratoconus: a condition that causes irregular corneal shape and thinning of the corneas.
- Keratitis: this common but painful inflammation of the cornea can often lead to swelling and infection. Keratitis can be caused by a number of things including bacteria, fungi, and viruses.
- Fuchs’ dystrophy: a chronic medical condition that causes the innermost (endothelial) layer of the cornea to deteriorate. This corneal disease accelerates with age, initially presenting itself as a blurriness that clears up throughout the day, but eventually manifests in persistent hazy vision and even corneal blisters.
- Corneal damage from previous eye surgeries
- Corneal damage from trichiasis, a condition wherein eyelashes grow inward
Infections can spring up from anything as innocuous as a small corneal scratch. Make sure you know your scratched cornea symptoms so that you can get treatment before a minor problem turns into a major one.
Corneal transplant recovery
During a transplant the cornea is, to some extent, fully removed (unlike LASIK, which requires just the healing of the corneal flap), so recovery time will vary greatly in correspondence with the type of transplant performed. The less invasive the procedure the quicker the recovery time; a patient can recover from endothelial keratoplasty in just a few weeks while penetrating keratoplasty takes much longer.
Full thickness corneal transplant recovery can take up to a year or longer. You will be able to return to normal activities much sooner – usually within a few weeks – but your eye will take some time to accept its new cornea. You will be prescribed steroid eye drops as well as other necessary medications to help mitigate infection and discomfort. As with any other eye surgery, there are a few things to avoid doing until your doctor gives you the go-ahead, such as driving, exercising, and swimming.
What risks come with corneal transplants?
Corneal transplants, while generally safe and effective, present the possibility of rejection of the graft. This happens because your body’s immune system believes the donated tissue to be a foreign substance and attempts to destroy it. Organ rejection, if detected early enough, is often reversible.
Consummate communication with your doctor during your recovery can help ease your recovery and might even save your new cornea. Here are some signs that your body might be rejecting the graft:
- Excessive pain and irritation
- Blurred or clouded vision
- Light sensitivity
- Red eyes
- Bleeding
Risks, while inherent in any surgical procedure, are a major reason to work with a doctor that you can trust.
Think You May Need a Corneal Transplant? Speak to an Expert at Eye Center of Texas.
When is a corneal transplant necessary? There are a multitude of reasons why your ophthalmologist would recommend a corneal transplant as the best course of action to either relieve pain or correct vision, but only they can tell you.
Our surgeons at Eye Center of Texas, like cornea specialist Dr. Yasir Ahmed, are at the forefront of surgical and clinical techniques, all in service of giving you the safest and quickest route to comfortable, clear vision.
If you are wondering who is a candidate for corneal transplant call us at 713-797-1010 or request an appointment online to find out what solutions will work for your vision.
More Helpful Articles by Eye Center of Texas:
Related Articles
Financing Options Available
Apply today to find a financing option that meets your needs.
Our Locations
Houston/Bellaire
6565 W. Loop S., Suite 650Bellaire, TX 77401
Medical Office:
713-797-1010
Medical Fax:
713-357-7276
LASIK/Near Vision:
Office: 713-395-1515
Fax: 713-357-7278
Pasadena
4415 Crenshaw RoadPasadena, TX 77504
Medical Office:
281-977-8800
Medical Fax:
281-977-8877
Sugar Land
15200 S.W. Freeway, Suite 130Sugar Land, TX 77478
Medical Office:
281-277-1010
Medical Fax:
281-277-4504
Clear Lake
455 E. Medical Center Blvd., Suite 110Webster, TX 77598
Medical Office:
281-332-1397
Medical Fax:
281-282-9152
Katy
Greenhouse Medical Plaza2051 Greenhouse Road, Suite 110
Houston, TX 77084
Medical Office:
346-547-7070
Medical Fax:
281-214-2971
The Woodlands/Conroe
100 Medical Center Blvd., Suite 118Conroe, TX 77304
Medical Office:
936-647-1610
Medical Fax:
936-647-1620