Medically Reviewed by:
Can Macular Degeneration Be Cured?
Age-related macular degeneration (AMD) is one of the most common causes of vision loss in older adults. However, not everyone who develops this condition will experience severe changes to their vision, especially at first.
When in more advanced stages, those with macular degeneration can have more trouble seeing objects directly in front of them and have significantly compromised night vision. There is no cure for AMD, but there are treatments that can slow the progression of the condition.
Keep reading to learn more about macular degeneration and the treatments available to slow or stop vision loss!
Related Articles
Medically Reviewed by:
New Year, New Vision: 9 Houston Spots that Come into Crystal Clear Focus in 2025 Post-LASIK
There has never been a better time to consider LASIK vision correction. LASIK is one of the most popular laser vision correction procedures in the United States.
Millions of people have chosen this simple, effective option for clearer, sharper vision without glasses or contacts. The end of the year is coming, which means you can use your holiday break to give yourself the
gift of clear vision without the hassle of glasses or contacts.
By the beginning of the new year, you’ll be ready to get out and enjoy the best activities Houston has to offer after LASIK!
Related Articles
Medically Reviewed by:
What is EVO ICL, and is it Right for You?
Not everyone who wants laser vision correction is a good candidate for LASIK. While it is an extremely popular procedure, it is not right for everyone due to several factors such as prescription needs, eye anatomy, or personal preference.
The good news is that there are other vision correction options available. One option that can work well for people who are not good candidates for LASIK is the EVO ICL.
The EVO ICL is an implantable Collamer lens that can offer improved vision and reduce your need for glasses and contact lenses. Keep reading to learn more about the EVO ICL, including whether it may be right for you!
Related Articles
Medically Reviewed by:
Why LASIK Might Be Your Ticket to Visual Freedom this Holiday Season
The holiday season will be here before you know it. If you’ve been thinking about giving yourself the gift of a laser vision correction procedure, this is the perfect time to get started.
Millions of people have chosen LASIK to correct their vision. After all, how could you say no to finally cutting the cord from glasses and contacts?
With a short recovery time, you can plan to have LASIK this fall and begin the holiday season with sharp, clear eyesight. Keep reading to discover why LASIK might be your ticket to visual freedom this holiday season!
Related Articles
Medically Reviewed by:
Here’s Why Choosing the Light Adjustable Lens in Houston Could Change Your Life and Vision
Do you have cataracts? They are among the most common causes of visual changes, especially among older adults.
Most people will develop age-related cataracts that will cause vision changes or vision loss. The only way to treat cataracts is with cataract surgery, which is why cataract surgery is one of the most common procedures you can undergo.
When you’re ready for cataract surgery, you’ll have a choice of which type of intraocular lens (IOL) you want to replace the clouded natural lens of your eye. IOLs ensure you can see clearly after cataract surgery and can also address other visual issues, such as refractive errors or presbyopia.
Many people choose premium IOLs like the Light Adjustable Lens for the best vision correction after cataract surgery. Keep reading to discover why choosing the Light Adjustable Lens in Houston could change your life and vision!
Related Articles
Medically Reviewed by:
How Do You Know When to Have Cataract Surgery?
Cataracts are among the most common causes of vision changes as you age. Age-related cataracts can cause symptoms like blurry vision, difficulty seeing in low light, and cloudy patches in your field of vision.
The only way to treat cataracts is with cataract surgery. Although it may sound daunting, it does not have to be. Cataract surgery can be life-changing for many patients, allowing them to resume activities and they feel more confident! Keep reading to find out how to know when to have cataract surgery!
Related Articles
Medically Reviewed by:
Macular Degeneration Symptoms
Macular degeneration is an eye condition that affects the macula, the central part of the retina responsible for sharp, central vision. As this disease progresses, it can lead to a gradual or sudden loss of central vision, making it difficult to perform activities that require detailed sight, such as reading, driving, or recognizing faces.
One of the earliest and most common symptoms of macular degeneration is blurred or distorted central vision. You may notice that straight lines appear wavy or bent or that there are blank spots or dark areas in your central field of vision. Additionally, colors may appear dull or faded.
Other common macular degeneration symptoms include:
- Difficulty adapting to low-light conditions
- Increased sensitivity to glare and bright lights
- Difficulty recognizing faces or reading fine print
As the disease advances, these symptoms may become more pronounced, and you may experience a significant loss of central vision, leaving only peripheral vision intact.
In this blog post, we’ll dive deeper into the various symptoms of macular degeneration, how to recognize them, possible treatments for macular degeneration, and what steps you can take to manage this condition and preserve your remaining vision.
1. Blurred or distorted central vision
Distorted or sudden blurry vision is often one of the earliest noticeable symptoms of macular degeneration. Objects that you’re looking at directly may appear fuzzy, hazy, or lacking in detail and definition.
Additionally, distortion of central vision can cause straight lines to appear bent, curved, or wavy. This distortion can make things look misshapen or warped when viewed directly ahead. Blurred and distorted central vision can significantly impact daily activities and serve as an early warning sign that macular degeneration may be developing.
2. Blank spots or dark areas in the central field of vision
One concerning symptom of macular degeneration is the appearance of blank spots or dark areas in the central field of vision. As the macula degenerates, it can lead to localized areas of vision loss or impairment.
Individuals may notice blind spots or empty patches directly ahead where vision seems to be missing or blacked out. These blind spots can make it difficult to see things that are directly in front of you, as parts of the image essentially have holes or dark smudges obscuring them.
The size and location of these blank areas can vary, but they typically affect the central vision used for activities like reading, watching TV, or recognizing faces and fine details.
While blind spots can start small, they may grow larger as macular degeneration progresses. Noticing these new blank spots or dark areas should prompt an urgent visit to a macular degeneration doctor in Houston for evaluation.
3. Colors appearing dull or faded
As macular degeneration progresses, it can cause colors to appear dull, faded, or less vibrant than normal. The macula contains a high concentration of cone cells, which are photoreceptors responsible for color vision and the perception of fine detail. So, when the macula deteriorates due to age-related macular degeneration, it impacts the functioning of these cone cells.
As a result, colors may start to look muted, washed out, or lacking in richness compared to how they appeared previously. Vibrant hues can seem lackluster, and it may become difficult to discern subtle variations in color tone or shade. Additionally, colors can take on a brownish tint as the ability to perceive blue/violet light diminishes.
4. Difficulty adapting to low-light conditions
The macula plays a crucial role in enabling our eyes to adjust and function properly in varying levels of light. So, as the macula degenerates, it can impair the eye’s ability to transition and adapt smoothly when moving between brightly lit and dimly lit environments. This light adaptation issue can make it challenging to see clearly and discern details after entering a darker area from bright sunshine or an illuminated room. The eyes may struggle to adjust, leaving the person essentially “blind” for several long moments until their remaining photoreceptor cells can eventually catch up.
In some cases, the difficulty adapting to low lighting can also cause halos or glare to appear around light sources, further exacerbating the problem. This symptom can lead to feelings of clumsiness, lack of confidence, and increased risk of falls or missteps when navigating unfamiliar low-light areas. Early detection is key to implementing strategies to cope with this challenging aspect of age-related macular degeneration (AMD) eye disease.
5. Increased sensitivity to glare and bright lights
As the macula deteriorates, it impairs the eye’s ability to filter intense light sources. Bright sunlight, harsh interior lighting, or reflective glare can suddenly feel intensely bright and blinding.
This heightened sensitivity stems from the breakdown of the macula’s protective filters that normally shield the retina. Attempting activities in overly bright conditions induces temporary blindness, making it difficult to see.
Managing this symptom requires sunglasses, anti-glare filters, and controlling environmental brightness. Early recognition allows the implementation of coping techniques to preserve the remaining vision.
6. Difficulty recognizing faces or reading fine print
Difficulty recognizing faces or reading fine print is a frustrating symptom that many individuals with wet or dry macular degeneration experience. As we’ve mentioned, the macula is responsible for our central vision — the sharp, straight-ahead sight needed for tasks that require focusing on fine details.
As macular degeneration progresses, it can significantly impair the ability to discern the intricate features that allow us to easily distinguish one face from another. Facial attributes like eyes, noses, and mouths may appear blurred or distorted, making it challenging to recognize even close friends or family members.
Similarly, reading can become an arduous task, as the tight spacing and small lettering of books, magazines, and computer screens can become increasingly illegible.
7. Gradual or sudden loss of central vision
For some individuals, the loss of central vision occurs gradually over time. They may first notice blurred or distorted sight in the middle of their field of view. This can slowly progress to larger blank spots or blind areas until only peripheral side vision remains intact.
However, in other cases, central vision loss can occur rapidly and seemingly out of the blue. One day, they have normal sight, and the next, they are struck with a substantial impairment in their ability to clearly see what is directly in front of them.
Whether gradual or sudden, prompt medical treatment is crucial when this core vision symptom first appears in order to try to preserve remaining sight.
Can anything be done for macular degeneration?
Yes, there are treatments available that can help slow the progression of macular degeneration and potentially prevent further vision loss, though the condition cannot be fully cured or reversed. Some of the treatment options include:
- Anti-VEGF Injections: For wet (neovascular) age-related macular degeneration, injections of anti-VEGF drugs like ranibizumab (Lucentis), bevacizumab (Avastin), or aflibercept (Eylea) into the eye can help stop abnormal blood vessel growth and leakage which damages the macula. (Learn more about the newest dry macular degeneration treatments)
- Laser Therapy: Certain types of “cold” laser treatments, like photodynamic therapy, can help slow leakage from abnormal blood vessels in wet macular degeneration.
- Nutritional Supplements: For dry macular degeneration, specific high-dose formulations of antioxidant vitamins and minerals like the AREDS/AREDS2 supplements have been shown to reduce the risk of progression.
- Low Vision Aids: While not treating the disease itself, low vision devices like magnifiers, bright lighting, or text-to-speech software can help maximize remaining vision.
- Lifestyle Changes: Quitting smoking, exercising regularly, and eating a diet rich in leafy greens and fish may help reduce AMD risk and progression.
Early detection is key, as vision lost to late-stage macular degeneration cannot be restored. However, prompt treatment can often delay or minimize further central vision loss in many cases.
Continue reading: Which is worse: wet or dry macular degeneration?
Experiencing macular degeneration symptoms? Call Eye Center of Texas today!
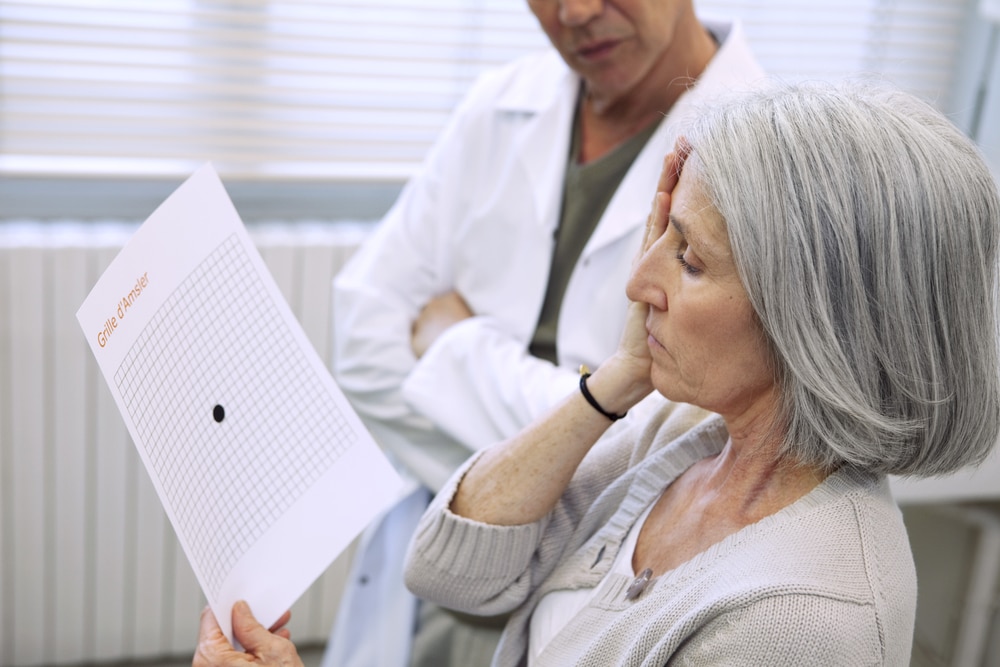
Macular degeneration can cause symptoms like blurred central vision, distorted sight, blind spots, and difficulty recognizing faces or reading fine print. If you are experiencing any changes to your vision, especially in your central field of view, or have an abnormal Amsler grid, it’s crucial to get your eyes examined promptly by an ophthalmologist.
At Eye Center of Texas, our experienced eye surgeons utilize the latest diagnostic technologies to detect macular degeneration as early as possible and provide personalized treatment plans to help preserve your vision for as long as possible. With convenient locations throughout Texas (including Houston/Bellaire, Pasadena, Sugar Land, Clear Lake, Katy, and The Woodlands/Conroe), we make it easy to access top-quality macular degeneration care in your area.
Don’t delay if you notice any potential macular degeneration symptoms. Request an appointment with our ophthalmologists today to take the next steps toward safeguarding your precious vision.
More Helpful Articles by Eye Center of Texas:
- What is the Average Age for Cataract Surgery?
- Pros and Cons of Photorefractive Keratectomy Surgery
- LASIK Surgery Age Limit
- What to do About Double Vision After Cataract Surgery
- Why is My Eyesight Getting Worse?
Related Articles
Medically Reviewed by:
What Are the Most Common Problems After Cataract Surgery?
Cataract surgery is a highly effective procedure that restores vision in individuals suffering from the clouding of the eye’s natural lens. While most patients experience no complications and enjoy a significant improvement in their eyesight, some side effects can occur after surgery. In this article, the cataract surgeons from Eye Center of Texas will explore the answer to the question “What are the most common problems after cataract surgery?” by examining some of the typical side effects, including:
- Mild discomfort and itching
- Cloudiness and/or blurry vision
- Light sensitivity
- Specks or floaters in vision
- Swelling
- Eye infection
Continue reading for insight into what patients might expect following cataract surgery in Houston and advice on managing these side effects effectively.
Continue reading about cataracts:
What are cataracts?
What causes cataracts?
1. Mild discomfort and itching after cataract surgery
Mild discomfort and itching are among the most common and immediately noticeable problems after cataract surgery, because it is natural for the eye to feel slightly irritated while it heals. Patients are strongly advised against rubbing or pressing on their eye, as this can exacerbate the irritation and potentially lead to complications.
To manage these symptoms, your surgeon may recommend over-the-counter pain relievers and prescribe eye drops to reduce inflammation and prevent infection. Typically, these discomforts diminish significantly within a few days post-operation, but it’s crucial to follow your surgeon’s care instructions closely and report any severe or lasting symptoms immediately.
2. Cloudiness and/or blurry vision after cataract surgery
Cloudiness and/or blurry vision after cataract surgery is a prevalent concern among patients, but in many cases, cloudiness or blurry vision may not be a side effect from the cataract surgery at all.
Rather, it may be the result of your eye getting used to its new lens. This phenomenon typically stems from the natural adjustment of the eye to the new intraocular lens (IOL) implanted during the procedure or from slight swelling of the cornea. Most patients state that their vision becomes less cloudy only 48 hours post-op but keep in mind, if you have floaters, they may be more visible now that you are seeing through a clear lens.
Typically, patients who opt for Monofocal IOLs (the standard IOL that’s covered by most insurances) can expect a slightly longer time before adjusting to their new vision. This is because Monofocal lenses only correct nearsightedness or farsightedness, but not both.
Patients typically opt to correct for nearsightedness (for seeing far away objects) and then rely on glasses to help them see objects which are close-at-hand.
3. Sensitivity to light after cataract surgery
Sensitivity to light after cataract surgery is another common symptom that patients may experience during cataract surgery recovery. This condition, known as photophobia, usually dissipates a few days following the procedure as the eye heals. During this time, the pupil is adjusting to the new intraocular lens and the increased clarity of vision, which can lead to an increased sensitivity to bright lights or glare.
Wearing sunglasses when outdoors and avoiding harsh indoor lighting can help manage this sensitivity effectively. It’s also beneficial to use artificial tears if the eyes feel dry or irritated, as this can sometimes exacerbate sensitivity to light.
Over time, as the eye adapts to the IOL and recovers from surgery, light sensitivity should markedly decrease. However, if severe light sensitivity persists, it’s essential to consult with your surgeon, as it may indicate underlying issues that need attention.
4. Specks or floaters in vision after cataract surgery
Seeing specks or floaters in your vision after cataract surgery can be alarming, but it’s often not a cause for concern. These small, dark shapes or lines may appear to drift across your field of vision and are commonly caused by tiny bits of protein or debris trapped in the vitreous, the gel-like substance that fills the eye.
After cataract surgery, these particles can become more noticeable as they move around inside the eye due to changes in pressure during the procedure. In most cases, these floaters will eventually settle and become less bothersome. However, if they persist or increase in number over time, it’s important to consult with your doctor as it may indicate a more serious issue such as inflammation or bleeding within the eye.
5. Swelling after cataract surgery
Swelling of the eye area is a common reaction following cataract surgery, typically manifesting as puffiness around the eyelids or within the eye itself. This occurs as the body’s response to the surgical intervention and the healing process that follows.
To alleviate swelling, patients are advised to use cold compresses gently applied to the affected area and to keep their head elevated, especially during sleep, to reduce fluid accumulation. Additionally, your surgeon may prescribe anti-inflammatory medication or eye drops to help manage swelling and discomfort. Usually, the swelling diminishes significantly within the first few days post-surgery, but in some cases, it may take a couple of weeks to fully resolve.
Like most side effects after cataract surgery, continuous monitoring of the swelling is crucial; if it worsens or is accompanied by severe pain or vision changes, immediate medical attention should be sought as it could indicate complications requiring prompt treatment.
6. Eye infection after cataract surgery
While infections following cataract surgery are rare, they represent a serious potential complication. The primary concern is endophthalmitis, an inflammation of the interior of the eye caused by infection, which can lead to significant vision loss if not treated promptly and effectively.
Symptoms of an eye infection can include severe pain, redness, blurred vision, and discharge from the eye. To minimize the risk of infection, patients must adhere to post-operative care instructions meticulously, such as using prescribed antibiotic eye drops, avoiding rubbing or touching the eye, and keeping water away from the eye during the initial healing period.
While in most cases infections can be managed effectively and risks can be mitigated, you’ve got to act fast, because infections can become dangerous quickly.
What to expect: cataract recovery timeline
The recovery timeline for cataract surgery and laser cataract surgery procedures varies from patient to patient, but typically patients start to notice an improvement in their vision within a few days after the procedure. However, it’s important to note that complete healing can take up to 3-6 weeks.
During the initial weeks of recovery, patients may experience fluctuations in their vision or mild discomfort, which gradually subsides over time. Outside of initial blurriness and dry eyes, side effects and problems after cataract surgery are infrequent and rarely threatening.
First 24 to 48 hours post-surgery
During the first day or two after surgery, it’s common for patients to have blurry vision as the eye starts to heal and adjust. It’s essential during this period to rest the eyes and avoid any strenuous activities or heavy lifting, which could strain the eyes and impact the healing process.
First week post-surgery
Most patients find that their vision significantly improves within the first week after surgery. It’s crucial to continue following the post-operative care instructions provided by the ophthalmologist, including using the prescribed eye drops to prevent infection and reduce inflammation.
Six weeks post-surgery
By the six-week mark, most patients have fully recovered from cataract surgery and have stable vision. Throughout the recovery period, even after your vision has stabilized, wearing sunglasses to protect your eyes from bright lights and UV rays is recommended, at least until you’ve had a chance to follow up with your ophthalmologist. It’s important to have a follow-up appointment with your ophthalmologist to ensure the eye is healing correctly and to assess if any further treatment is needed.
What to expect from cataract surgery at Eye Center of Texas
What are the most common problems after cataract surgery? Most of the common issues that arise after cataract surgery are standard-issue for the recovery process. While the recovery process from cataract surgery is notably smooth and quick for the majority, it’s essential to keep an eye out for the most common problems after cataract surgery, so that you can address any complications as they arise.
Having performed over 80,000 successful cataract surgeries in our facilities across Texas (including Houston/Bellaire, Pasadena, Sugar Land, Clear Lake, Katy, and The Woodlands/Conroe), the surgeons of Eye Center of Texas have transformed the lives of thousands of patients and can help answer any questions you have about the process.
Put your vision in the hands of nationally renowned blade-free cataract surgery surgeons, and request an appointment online today to get started on your journey to better vision.
More Helpful Articles by Eye Center of Texas:
- What is the Average Age for Cataract Surgery?
- Pros and Cons of Photoreactive Keratectomy
- LASIK Surgery Age Limit
- Why is My Vision Getting Worse?
- Patients Say We Are the Best Ophthalmologists in Houston
Related Articles
Medically Reviewed by:
What is the Average Age for Cataract Surgery?
Whether you’re approaching your forties or fifties and are concerned about developing cataracts in the future, or you’re 60+ and you’ve begun to notice problems with your vision, you may be asking yourself “What is the average age for cataract surgery?” Or, more importantly, “When should I have cataract surgery?”
While many people can develop cataracts as early as their forties, prevailing data suggests that the average age for cataract surgery is around 65. In this article, we will look at some of the data surrounding when and why people opt for cataract surgery, early signs of cataracts, and what to expect when you make your appointment.
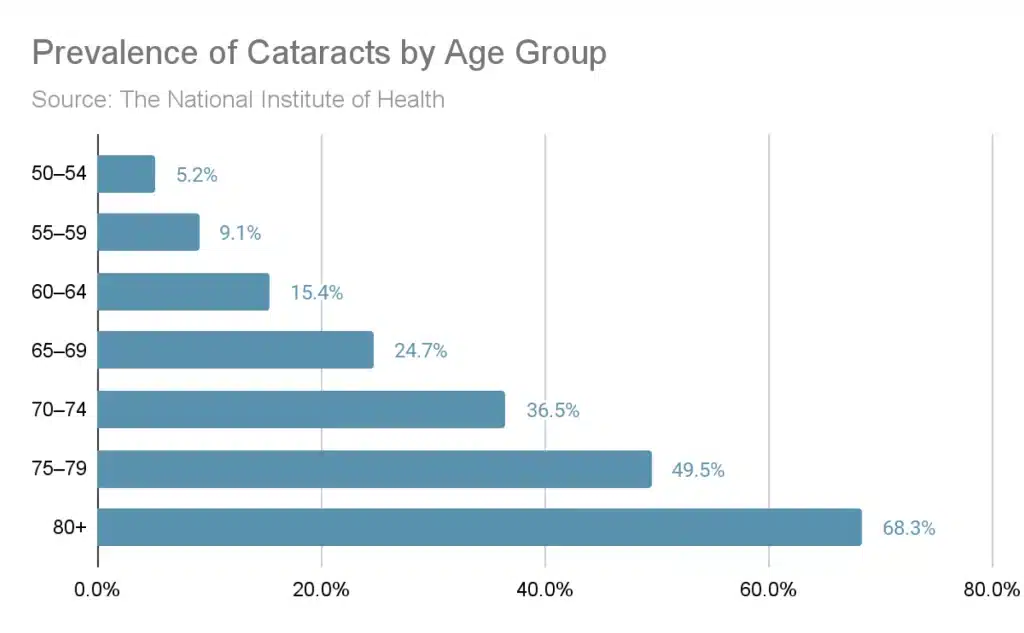
Prevalence of cataracts by age
Roughly 90% of people will develop cataracts by the age of 65. Like other age-related degenerative conditions, the chance of cataracts occurring only increases the older a person gets. Per the National Institute of Health, the prevalence of cataracts by age rapidly increases with every decade of life. This means that the likelihood of needing cataract surgery at age 60 or cataract surgery after 70 is far higher than seeing a doctor about your cataracts at age 50.
What is the youngest age for cataract surgery?
Because cataracts develop over time and tend to affect older people more than they affect younger people, surgery may not be required for younger people in the early stages. And while it’s certainly never too early to get cataract surgery, waiting too long can greatly reduce the procedure’s effectiveness.
Many people who are younger than the average age for cataract removal, say in their forties and fifties, may put off getting surgery for their cataracts for a number of reasons. Maybe the cataracts don’t greatly affect their vision or quality of life, or maybe they’re worried their cataracts will return after the procedure. If you or a loved one is wondering, “Can cataracts come back after surgery?” you’ll be relieved to know that the answer is no.
Because there’s no risk of cataracts returning post-surgery, is it better to have cataract surgery early for several reasons. First, getting cataract surgery earlier in life means clearer vision later in life. Rather than dealing with increasingly cloudy vision as you age into your golden years, you can make the choice to get surgery early and maintain your quality of life and independence.
Additionally, although the procedure is short and relatively noninvasive, healing from surgery tends to be easier and faster for younger people than it is for older people.
Continue reading: Can you wait too long to have cataract surgery?
How do you know when it’s time for cataract surgery?
Sooner or later, nearly everyone will develop cataracts as they age into their sixties and seventies. And if you were wondering whether there is a non-surgical, natural remedy for cataracts, there isn’t one. You’ll know when it’s time for cataract surgery by reviewing the following questions:
Are my cataracts making my life difficult?
Cataracts can significantly impact quality of life by causing blurred vision, difficulty reading, and reduced ability to drive safely. They can also affect daily activities where vision is important, but often taken for granted. For example, something as simple as cooking dinner can become challenging due to impaired depth perception and foggy vision. Watching television or enjoying hobbies like painting can become frustrating due to decreased visual clarity.
If left untreated, cataracts can also impact other, more serious aspects of life. They could lead to an increased risk of falls and accidents, particularly in dimly lit environments. They can also make recognizing friends and loved ones more challenging, or increase eye strain at work.
Do I have a hard time seeing at night?
Cataract-related difficulty seeing at night can significantly affect one’s safety and quality of life. Impaired night vision increases the risk of accidents, especially while driving or navigating in low-light environments. Since nighttime visibility is crucial for many activities and responsibilities like driving or even moving around the house safely, cataract-related vision problems can severely limit independence and confidence.
If you’re having difficulty seeing at night due to cataracts, treatment might be the next logical step. By removing the cloudy lens and replacing it with a clear artificial lens, cataract surgery improves night vision, enhancing safety and allowing individuals to resume their normal activities with greater ease and confidence.
Am I sensitive to glare?
Cataracts can cause sensitivity to light and glare due to the changes they induce in the eye’s lens. As cataracts develop, the normally clear lens becomes cloudy, resulting in light scattering inside the eye. This scattering of light causes increased sensitivity to bright lights and glare.
As a result, individuals with cataracts may find it challenging to tolerate bright environments, leading to avoidance of outdoor activities or difficulty driving at night due to the intense glare from oncoming headlights. Cataract surgery often resolves this sensitivity by replacing the cloudy lens with a clear artificial lens, restoring the eye’s ability to properly focus light onto the retina and reducing sensitivity to light and glare.
Are there vision differences between my eyes?
In some cases, cataracts may develop at different rates in each eye, leading to variations in visual acuity between them. One eye might have a more advanced cataract, resulting in more significant vision impairment compared to the other eye.
The location and severity of cataracts within each eye can vary. If a cataract is located in the central part of the lens in one eye but more peripherally in the other, it can lead to differences in visual clarity and focus. Moreover, factors such as astigmatism or pre-existing differences between the eyes can worsen the discrepancy in vision caused by cataracts.
Addressing disparate levels of vision due to cataracts may require customized treatment plans, such as cataract surgery tailored to the specific needs of each eye, to achieve balanced and optimized vision between the two eyes.
Eye Center of Texas is ready to answer all of your cataract surgery questions
Now that we’ve discussed the average age for cataract surgery, if you have cataracts, but you’re not at the average age for cataract removal, you can still benefit from setting up an appointment with an eye surgeon. Cataract surgery is a fast and relatively pain-free procedure that can dramatically improve both your vision and your overall quality of life.
The acumen of our cataract surgeons speaks for itself. Our Houston cataract surgeons — such as Dr. Mark L. Mayo, Dr. Yasir Ahmed, and Dr. Edward C. Wade — have completed thousands of successful cataract procedures, and left thousands of patients happy.
Put your eye care into the hands of surgeons you can trust at Eye Center of Texas. We offer cataract surgery at our locations throughout Texas including Houston/Bellaire, Pasadena, Sugar Land, Clear Lake, Katy, and The Woodlands/Conroe. Request an appointment today to see if you are a candidate!
More Helpful Articles by Eye Center of Texas:
- How Old Do You Have to Be to Get LASIK?
- What To Do About Double Vision After Cataract Surgery
- Why Is My Vision Getting Worse?
- Why Patients Say We Are the Best Ophthalmologists in Texas
- 7 Things To Do When Preparing for LASIK Surgery
Related Articles
Medically Reviewed by:
Pros and Cons of Photorefractive Keratectomy
For many patients, the dream of clear vision without the hassle of glasses or contact lenses may be a reality thanks to advancements in vision correction procedures like photorefractive keratectomy (more commonly known as PRK or PRK LASIK).
Photorefractive keratectomy, or PRK, is a safe and effective alternative to LASIK surgery, for those who don’t qualify as candidates for LASIK. However, as with any medical procedure, there are things to consider when deciding if PRK eye surgery is right for you.
The ophthalmologists at Eye Center of Texas are here to shed light on the PRK eye surgery pros and cons, what to expect during the surgery and recovery, and who might and might not be an ideal candidate. We’re hoping that this will help you to make an informed choice for your ocular health.
| Photorefractive Keratectomy Pros | Photorefractive Keratectomy Cons |
|
|
What is PRK surgery?
Photorefractive keratectomy (PRK) is a type of refractive surgery that can correct common vision problems such as mild to moderate nearsightedness, farsightedness, and astigmatism. The PRK procedure itself is fairly short, lasting only around 15 minutes long. The surgery reshapes the cornea, the clear front part of the eye, so that light is focused properly onto the retina.
The difference between PRK and LASIK is that unlike LASIK, which creates a flap in the cornea, PRK gently removes the outer layer of the cornea before reshaping it with an ultraviolet beam of light. Once the cornea is reshaped, a “bandage” contact lens is placed over the eye to help protect the surface as it heals. The top layer of the cornea eventually grows back over the reshaped internal layers.
Want to know if PRK eye surgery is the best vision correction procedure for you? Let’s discuss the PRK eye surgery pros and cons.
What are the advantages of photorefractive keratectomy?
Here is a list of reasons why getting PRK may be beneficial for you and your vision.
1. PRK is typically safer than LASIK
Is PRK surgery safe? Yes! Since PRK does not leave a flap in your cornea like LASIK does, you are less likely to deal with complications such as flap displacement, wrinkling, or unexpected growth.
PRK is seen as safer for patients who have:
- Dry eye condition
- Active lifestyle preferences
- High corrective prescription (meaning you are more farsighted)
- Thin corneas
How safe is photorefractive keratectomy?
While every medical procedure has its risks, such as infection or miscorrection, PRK is considered a low-risk procedure when performed by a skilled eye surgeon. Because PRK does not require anesthesia, many patients worry about pain, but there’s no need to be anxious. Your ophthalmologist will use numbing drops in your eyes before the procedure and offer an oral sedative if you feel you need it. Many patients note that PRK is quick and painless.
2. More patients qualify for PRK
A big reason that not many people qualify for LASIK is that their corneas are too thin or they deal with dry eye syndrome as stated above. However, patients with thin corneas or corneal irregularities that may complicate the flap creation from LASIK could benefit from PRK instead.
Additionally, PRK can be a suitable option for people with certain professions or hobbies that may involve contact sports or other activities where contact with the eyes is possible.
How do I know if I qualify for PRK? Here is a list of indicators that you would be an ideal candidate for PRK:
- You’re at least 18 years old
- You experience refractive errors (myopia, hyperopia, astigmatism)
- You’re not pregnant or nursing
- You’ve had a stable prescription for at least one year
- You haven’t experienced eye injuries or infection within the last year
- You’re not suffering from dry eye syndrome
- You have no issues with keratoconus
Who is a bad candidate for PRK?
Certain health and lifestyle factors could make PRK a less-than-ideal choice for vision correction surgery. Candidates who do not qualify for PRK may include:
- People with an unstable prescription
- People with a history of corneal diseases
- People with systemic health conditions (especially those affecting the immune system)
- Individuals with unrealistic expectations about the results and recovery process
3. Fewer risks and side effects
PRK has fewer and less severe side effects than a surgery like LASIK. For example, you won’t run the risk of getting dry eye syndrome from disrupted nerves. However, every vision correction surgery will come with its own set of side effects to be aware of.
Common PRK side effects to keep an eye out for in the first week of recovery include:
- Mild to moderate discomfort or itching
- Light sensitivity
- Seeing bursts or halos of light for the first few weeks
- Cloudy or hazy vision (corneal haze)
4. High success rate
The PRK success rate is very high, making it a popular choice among patients. According to the FDA, about 95% of PRK patients achieve 20/40 vision without the need for corrective lenses or glasses after one-year post-op. This means that many patients can throw out their glasses or contacts within a year of getting PRK.
5. Long-term results
During the initial healing phase, the outer layer of the cornea regenerates, leading many ophthalmologists to believe that PRK offers a more stable and long-term outcome compared to LASIK. The gradual healing process also means that the vision may take longer to fully stabilize, but the results are often more predictable.
What are the cons of PRK surgery?
While photorefractive keratectomy may come with many benefits, it also is accompanied by a short list of things that all patients should consider before committing to PRK.
1. Longer recovery time
PRK recovery is a little longer than LASIK due to the nature of the surgery. Where the corneal flap can simply be realigned after LASIK, the outer layer that was scraped away during PRK needs time to grow back. Patients can expect to be fully recovered within 2-4 weeks of getting PRK, but recovery time may depend on the individual patient’s circumstances.
2. Discomfort and sensitivity
Due to the removal of the protective outer layer of the cornea during PRK, the initial days following the procedure can bring a little more discomfort than LASIK or other surgeries. Patients often experience some mild pain, light sensitivity, or hazy vision which generally subsides within a few days as the cornea begins to regenerate. Make sure to not do any strenuous exercise or activities while you’re in recovery.
3. Possibility of vision overcorrection or undercorrection
In the event that your vision was over or undercorrected during your surgery, you may need to go back to glasses or contacts or even get an additional surgery to remedy the problem. Although it is rare, there is a possibility that your vision could worsen after getting PRK. Being aware of these possibilities and speaking to your doctor about them will make the process a lot smoother.
4. Risk of infection
Because PRK requires removing the outer layer of the cornea which serves as a natural protective barrier, your eyes are slightly more vulnerable to infection post-PRK. However, this risk can be minimized greatly if you are diligent about your post-operative dos and don’ts.
PRK dos and don’ts:
Do:
- Follow up with your doctor
- Use your eye drops as prescribed
- Wear sunglasses to avoid bright lights
- Consult your doctor before and after your procedure about medications to help with possible discomfort
Don’t:
- Rub or touch your eyes
- Participate in strenuous activities
- Drive until you are safe to do so
- Swim
- Put on makeup or any cream products near your eyes
- Smoke
Is photorefractive keratectomy right for you? Ask the ophthalmologists at Eye Center of Texas.
Photorefractive keratectomy is a great surgical option for those who don’t want to wear glasses or contact lenses for the rest of their lives but don’t qualify for LASIK. With its safety, high PRK success rate, and high rate of patient satisfaction, PRK may also be the right choice for you.
The best way to determine if PRK is right for you is to schedule a consultation with an experienced eye surgeon. During this visit, your eyes will be thoroughly examined, and your surgeon will discuss your candidacy, potential risks, and what to expect throughout the process.
At Eye Center of Texas, our talented PRK surgeons including Dr. Yasir Ahmed, M.D., Dr. Mark Mayo, M.D., and Dr. Edward Wade, M.D., F.A.C.S. have helped countless patients get their desired vision with PRK. With their expertise, you can rest assured that your vision is in the best hands.
Ready to get started? We offer photorefractive keratectomy at our locations throughout Texas including Houston/Bellaire, Pasadena, Sugar Land, Clear Lake, Katy, and The Woodlands/Conroe. Request an appointment today to see if you are a candidate for PRK!
More Helpful Articles by Eye Center of Texas:
- How Old Do You Have to Be to Get LASIK?
- What To Do About Double Vision After Cataract Surgery
- Why Is My Vision Getting Worse?
- Why Patients Say We Are the Best Ophthalmologists in Texas
- 7 Things To Do When Preparing for LASIK Surgery
Related Articles
Financing Options Available
Apply today to find a financing option that meets your needs.
Our Locations
Houston/Bellaire
6565 W. Loop S., Suite 650Bellaire, TX 77401
Medical Office:
713-797-1010
Medical Fax:
713-357-7276
LASIK/Near Vision:
Office: 713-395-1515
Fax: 713-357-7278
Pasadena
4415 Crenshaw RoadPasadena, TX 77504
Medical Office:
281-977-8800
Medical Fax:
281-977-8877
Sugar Land
15200 S.W. Freeway, Suite 130Sugar Land, TX 77478
Medical Office:
281-277-1010
Medical Fax:
281-277-4504
Clear Lake
455 E. Medical Center Blvd., Suite 110Webster, TX 77598
Medical Office:
281-332-1397
Medical Fax:
281-282-9152
Katy
Greenhouse Medical Plaza2051 Greenhouse Road, Suite 110
Houston, TX 77084
Medical Office:
346-547-7070
Medical Fax:
281-214-2971
The Woodlands/Conroe
100 Medical Center Blvd., Suite 118Conroe, TX 77304
Medical Office:
936-647-1610
Medical Fax:
936-647-1620