Medically Reviewed by:
Can Macular Degeneration Be Cured?
Age-related macular degeneration (AMD) is one of the most common causes of vision loss in older adults. However, not everyone who develops this condition will experience severe changes to their vision, especially at first.
When in more advanced stages, those with macular degeneration can have more trouble seeing objects directly in front of them and have significantly compromised night vision. There is no cure for AMD, but there are treatments that can slow the progression of the condition.
Keep reading to learn more about macular degeneration and the treatments available to slow or stop vision loss!
Related Articles
Medically Reviewed by:
Macular Degeneration Symptoms
Macular degeneration is an eye condition that affects the macula, the central part of the retina responsible for sharp, central vision. As this disease progresses, it can lead to a gradual or sudden loss of central vision, making it difficult to perform activities that require detailed sight, such as reading, driving, or recognizing faces.
One of the earliest and most common symptoms of macular degeneration is blurred or distorted central vision. You may notice that straight lines appear wavy or bent or that there are blank spots or dark areas in your central field of vision. Additionally, colors may appear dull or faded.
Other common macular degeneration symptoms include:
- Difficulty adapting to low-light conditions
- Increased sensitivity to glare and bright lights
- Difficulty recognizing faces or reading fine print
As the disease advances, these symptoms may become more pronounced, and you may experience a significant loss of central vision, leaving only peripheral vision intact.
In this blog post, we’ll dive deeper into the various symptoms of macular degeneration, how to recognize them, possible treatments for macular degeneration, and what steps you can take to manage this condition and preserve your remaining vision.
1. Blurred or distorted central vision
Distorted or sudden blurry vision is often one of the earliest noticeable symptoms of macular degeneration. Objects that you’re looking at directly may appear fuzzy, hazy, or lacking in detail and definition.
Additionally, distortion of central vision can cause straight lines to appear bent, curved, or wavy. This distortion can make things look misshapen or warped when viewed directly ahead. Blurred and distorted central vision can significantly impact daily activities and serve as an early warning sign that macular degeneration may be developing.
2. Blank spots or dark areas in the central field of vision
One concerning symptom of macular degeneration is the appearance of blank spots or dark areas in the central field of vision. As the macula degenerates, it can lead to localized areas of vision loss or impairment.
Individuals may notice blind spots or empty patches directly ahead where vision seems to be missing or blacked out. These blind spots can make it difficult to see things that are directly in front of you, as parts of the image essentially have holes or dark smudges obscuring them.
The size and location of these blank areas can vary, but they typically affect the central vision used for activities like reading, watching TV, or recognizing faces and fine details.
While blind spots can start small, they may grow larger as macular degeneration progresses. Noticing these new blank spots or dark areas should prompt an urgent visit to a macular degeneration doctor in Houston for evaluation.
3. Colors appearing dull or faded
As macular degeneration progresses, it can cause colors to appear dull, faded, or less vibrant than normal. The macula contains a high concentration of cone cells, which are photoreceptors responsible for color vision and the perception of fine detail. So, when the macula deteriorates due to age-related macular degeneration, it impacts the functioning of these cone cells.
As a result, colors may start to look muted, washed out, or lacking in richness compared to how they appeared previously. Vibrant hues can seem lackluster, and it may become difficult to discern subtle variations in color tone or shade. Additionally, colors can take on a brownish tint as the ability to perceive blue/violet light diminishes.
4. Difficulty adapting to low-light conditions
The macula plays a crucial role in enabling our eyes to adjust and function properly in varying levels of light. So, as the macula degenerates, it can impair the eye’s ability to transition and adapt smoothly when moving between brightly lit and dimly lit environments. This light adaptation issue can make it challenging to see clearly and discern details after entering a darker area from bright sunshine or an illuminated room. The eyes may struggle to adjust, leaving the person essentially “blind” for several long moments until their remaining photoreceptor cells can eventually catch up.
In some cases, the difficulty adapting to low lighting can also cause halos or glare to appear around light sources, further exacerbating the problem. This symptom can lead to feelings of clumsiness, lack of confidence, and increased risk of falls or missteps when navigating unfamiliar low-light areas. Early detection is key to implementing strategies to cope with this challenging aspect of age-related macular degeneration (AMD) eye disease.
5. Increased sensitivity to glare and bright lights
As the macula deteriorates, it impairs the eye’s ability to filter intense light sources. Bright sunlight, harsh interior lighting, or reflective glare can suddenly feel intensely bright and blinding.
This heightened sensitivity stems from the breakdown of the macula’s protective filters that normally shield the retina. Attempting activities in overly bright conditions induces temporary blindness, making it difficult to see.
Managing this symptom requires sunglasses, anti-glare filters, and controlling environmental brightness. Early recognition allows the implementation of coping techniques to preserve the remaining vision.
6. Difficulty recognizing faces or reading fine print
Difficulty recognizing faces or reading fine print is a frustrating symptom that many individuals with wet or dry macular degeneration experience. As we’ve mentioned, the macula is responsible for our central vision — the sharp, straight-ahead sight needed for tasks that require focusing on fine details.
As macular degeneration progresses, it can significantly impair the ability to discern the intricate features that allow us to easily distinguish one face from another. Facial attributes like eyes, noses, and mouths may appear blurred or distorted, making it challenging to recognize even close friends or family members.
Similarly, reading can become an arduous task, as the tight spacing and small lettering of books, magazines, and computer screens can become increasingly illegible.
7. Gradual or sudden loss of central vision
For some individuals, the loss of central vision occurs gradually over time. They may first notice blurred or distorted sight in the middle of their field of view. This can slowly progress to larger blank spots or blind areas until only peripheral side vision remains intact.
However, in other cases, central vision loss can occur rapidly and seemingly out of the blue. One day, they have normal sight, and the next, they are struck with a substantial impairment in their ability to clearly see what is directly in front of them.
Whether gradual or sudden, prompt medical treatment is crucial when this core vision symptom first appears in order to try to preserve remaining sight.
Can anything be done for macular degeneration?
Yes, there are treatments available that can help slow the progression of macular degeneration and potentially prevent further vision loss, though the condition cannot be fully cured or reversed. Some of the treatment options include:
- Anti-VEGF Injections: For wet (neovascular) age-related macular degeneration, injections of anti-VEGF drugs like ranibizumab (Lucentis), bevacizumab (Avastin), or aflibercept (Eylea) into the eye can help stop abnormal blood vessel growth and leakage which damages the macula. (Learn more about the newest dry macular degeneration treatments)
- Laser Therapy: Certain types of “cold” laser treatments, like photodynamic therapy, can help slow leakage from abnormal blood vessels in wet macular degeneration.
- Nutritional Supplements: For dry macular degeneration, specific high-dose formulations of antioxidant vitamins and minerals like the AREDS/AREDS2 supplements have been shown to reduce the risk of progression.
- Low Vision Aids: While not treating the disease itself, low vision devices like magnifiers, bright lighting, or text-to-speech software can help maximize remaining vision.
- Lifestyle Changes: Quitting smoking, exercising regularly, and eating a diet rich in leafy greens and fish may help reduce AMD risk and progression.
Early detection is key, as vision lost to late-stage macular degeneration cannot be restored. However, prompt treatment can often delay or minimize further central vision loss in many cases.
Continue reading: Which is worse: wet or dry macular degeneration?
Experiencing macular degeneration symptoms? Call Eye Center of Texas today!
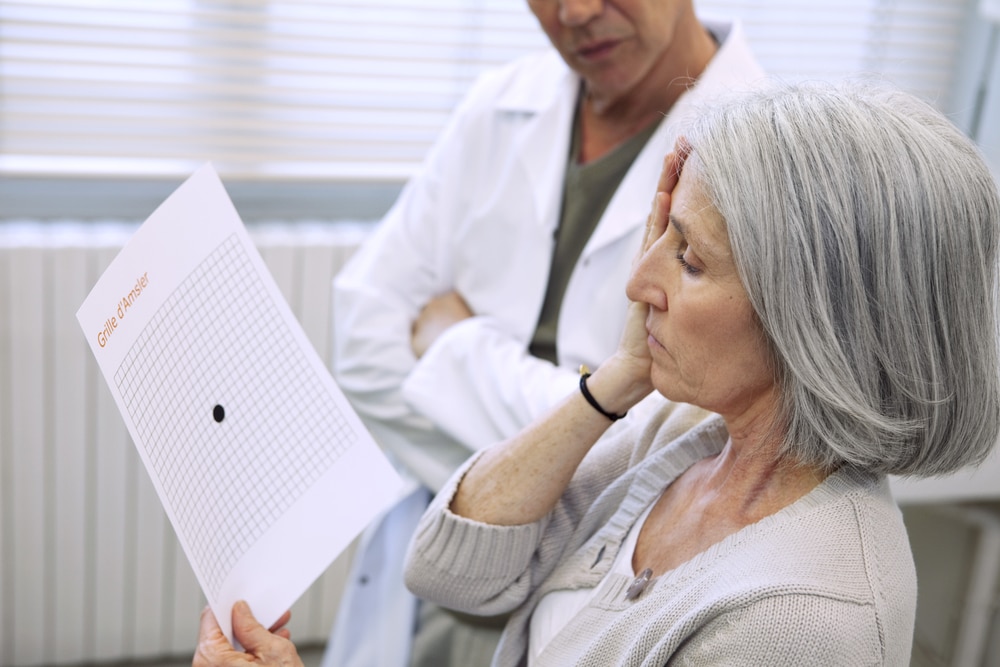
Macular degeneration can cause symptoms like blurred central vision, distorted sight, blind spots, and difficulty recognizing faces or reading fine print. If you are experiencing any changes to your vision, especially in your central field of view, or have an abnormal Amsler grid, it’s crucial to get your eyes examined promptly by an ophthalmologist.
At Eye Center of Texas, our experienced eye surgeons utilize the latest diagnostic technologies to detect macular degeneration as early as possible and provide personalized treatment plans to help preserve your vision for as long as possible. With convenient locations throughout Texas (including Houston/Bellaire, Pasadena, Sugar Land, Clear Lake, Katy, and The Woodlands/Conroe), we make it easy to access top-quality macular degeneration care in your area.
Don’t delay if you notice any potential macular degeneration symptoms. Request an appointment with our ophthalmologists today to take the next steps toward safeguarding your precious vision.
More Helpful Articles by Eye Center of Texas:
- What is the Average Age for Cataract Surgery?
- Pros and Cons of Photorefractive Keratectomy Surgery
- LASIK Surgery Age Limit
- What to do About Double Vision After Cataract Surgery
- Why is My Eyesight Getting Worse?
Related Articles
Medically Reviewed by:
What is the Latest Treatment for Dry Macular?
For far too long, individuals diagnosed with dry macular degeneration were faced with a daunting reality — there were essentially no cures and most treatment options were experimental. This degenerative condition of the eyes, which leads to progressive loss of vision, seemed to defy medical advancements, leaving patients in a disheartening situation.
However, the landscape of this condition has dramatically changed as of late when the Food and Drug Administration (FDA) gave its approval for a new treatment specifically targeting dry macular degeneration. So, what is the latest treatment for dry macular?
Pegcetacoplan, sold under the brand name Syfovre™, is a new treatment approved by the FDA. It’s a shot given inside the eye that might help slow down the worsening of geographic atrophy, a condition caused by advanced dry AMD.
But Syfovre™ isn’t the only new treatment for macular degeneration. Here’s what you need to know about the new dry AMD injections.
Can you stop the progression of dry macular degeneration?
Unfortunately, there is currently no cure for dry macular degeneration. However, the latest treatment options have shown promising results in slowing down the progression of this condition and preserving vision for longer.
For this reason, the earlier you see your ophthalmologist for common signs of macular degeneration, the earlier you can get a diagnosis and the more effective these treatments can be. Routine eye exams that include the Amsler eye grid test are crucial in catching this condition early on and starting treatment as soon as possible.
Once diagnosed, some of the common options for treatment include:
- Pharmacologic therapy treatments including Macugen, Lucentis, Avastin, and Visudyne Photodynamic Therapy
- Laser treatment
- Rheopheresis
- Low-dose radiation therapy
- Submacular surgery
- RPE transplant
- Macular translocation surgery
- Artificial vision
These were some of the only treatment options until the end of 2023. As we mentioned above, groundbreaking research has led to the approval of several new drugs for macular degeneration treatment, offering patients more options than ever before.
New treatments for dry macular degeneration
Let’s explore some of the most recent and promising treatments for dry macular degeneration that are revolutionizing the way ophthalmologists approach this condition.
Pegcetacoplan (Syfovre™)
Syfovre™, a product of Apellis Pharmaceuticals, represents a significant breakthrough in the management of dry AMD, with its active ingredient Pegcetacoplan designed to halt the disease’s progression.
This innovative treatment, administered through intraocular injection either monthly or bimonthly, has proven its efficacy in the treatment of geographic atrophy, a catastrophic outcome of age-related macular degeneration.
Safety and effectiveness validated by clinical trials
The safety and effectiveness of Syfovre™ were confirmed in two Phase III clinical trials. In these randomized, double-masked, sham-controlled trials, patients showed a significant reduction in macular lesions upon receiving the Pegcetacoplan injection either monthly or bimonthly, with more promising results seen in the monthly treatment group.
Two different trials, one involving 637 patients and another with 621 participants, both with advanced dry AMD, demonstrated the slowing of lesion growth in the macula. The more frequently administered treatment showed marginally better outcomes, further confirming the drug’s potential to slow the disease’s progression.
The results
The investigations reveal that the effectiveness of Pegcetacoplan increases over time. It not only decelerates the disease but also helps prevent further retinal degeneration. The emergence of Syfovre™ marks a significant milestone in the tireless efforts of doctors for macular degeneration to tackle this intricate disease and for patients whose quality of life has been affected by the vision loss that comes with geographic atrophy.
Avacincaptad Pegol (IZERVAY™)
At the end of 2023, the FDA approved yet another new treatment for macular degeneration known as IZERVAY™, formerly Zimura®. This drug, developed by Iveric Bio, provides yet another promising treatment option for the late-stage outcome of dry AMD known as geographic atrophy.
The active ingredient in IZERVAY™ is called Avacincaptad Pegol, which selectively blocks a protein called C5 that has been found to cause retinal cell damage in dry AMD. By doing so, it has the potential to slow down the progress of the disease and prevent further vision loss. It is the only therapeutical option on the market that can help protect healthy retinal cells by blocking the C5 protein.
IZERVAY™ is administered as an intraocular injection, given once every three months. This schedule offers patients a more convenient approach to managing their condition, compared to other treatments that require monthly injections.
Safety and effectiveness validated by clinical trials
Izervay’s effectiveness was demonstrated in rigorous clinical trials involving over 700 patients. The data from these trials showed a significant slowing of geographic atrophy progression by between 18-35% in one year in patients treated with IZERVAY™ when compared to those who were not treated.
The results
In addition to its primary benefits, Izervay has also been reported to be well tolerated by most patients. Some of the most common side effects include blurred vision, eye pain, and mild eye inflammation – all of which are manageable under the supervision of healthcare professionals.
Want to learn more about the newest dry macular degeneration treatments? Contact Eye Center of Texas today!
For those with loved ones or personal diagnoses of macular degeneration who constantly find themselves asking, “Are there any new treatments for dry macular degeneration?” We are overjoyed to tell you that yes, there are! So, what are the latest treatments for dry macular?
In 2023, the FDA approved two new drug options for patients suffering from the symptoms of dry AMD: Pegcetacoplan (Syfovre™) and Avacincaptad Pegol (IZERVAY™). The introduction of these drugs into the market represents a significant step forward in the field of ophthalmology and the fight against AMD.
With the continuous advancements in research and technology, we can only expect more innovative treatments to emerge in the future and Eye Center of Texas is here to ensure that our patients continue to have access to the best possible care options.
Whether you’re suffering from symptoms of wet vs. dry macular degeneration, are facing other macular conditions and need to explore macular pucker surgery, or are wondering if you’re a good candidate for either of these new treatments for macular degeneration, the ophthalmologists at Eye Center of Texas are here for you.
Contact us online to schedule an appointment at one of our locations in Houston/Bellaire, Pasadena, Sugar Land, Clear Lake, Katy, or The Woodlands/Conroe today!
More Helpful Articles by Eye Center of Texas:
- Why is There a Bump On My Eyelid?
- How to Find a Good Cataract Surgeon in Houston
- What to Look For to Find the Best LASIK in the World
- Where to Find the Best Cataract Surgery in Conroe, Texas
- Sudden Blurry Vision Causes
Related Articles
Medically Reviewed by:
What Causes Macular Degeneration?
What causes macular degeneration? Though the reason for the onset of macular degeneration is unknown, science has come a long way in understanding what is actually causing the symptoms of the disease. Here’s what science currently tells us about what causes macular degeneration, as well as macular degeneration warning signs to watch out for and more.
The current science behind what causes macular degeneration
Age-related macular degeneration (AMD) is an eye disease that primarily affects the central portion of the retina, known as the macula.
In its dry (non-neovascular) form –– the most common form –– little bits of fat and protein called drusen begin to collect underneath your retina. Individual drusen are typically harmless, but when they accumulate en masse behind your retina, they start to cut off the oxygen supply to your eye. In the wet (neovascular) form of macular degeneration, abnormal blood vessels (thought to form as an effort to rid your eye of drusen) also begin to form underneath the retina. Unfortunately, these blood vessels increase the risk of fluid or blood leaking into the retina.
Dry macular degeneration is considered less serious and causes more minimal vision loss than wet macular degeneration. Please see our article for more information regarding wet vs. dry macular degeneration.
FAQ: How long does it take to lose vision with macular degeneration?
On average, it takes approximately 10 years from diagnosis to become legally blind. In very severe cases, eyesight can be lost in as short as a few days. If you are near the age of 70, try to see your eye doctor regularly.
Macular degeneration risk factors
While what causes these drusen to collect (and thus what causes macular degeneration onset) is still unknown, several risk factors for AMD have been identified.
-
- Age: Age is by far the biggest determining risk factor for AMD. It’s very common for individuals over the age of 70 to be diagnosed with some degree of macular degeneration.
- Gender: Women are currently considered to be more likely to get AMD than men, but this may be because most women live longer than men. About ⅔ of all patients with AMD are women.
- Smoking: People who smoke have been found more likely to have AMD. It is thought that this is due to the fact that smoking reduces the amount of oxygen that reaches your eyes.
- High blood pressure: Like smoking, high blood pressure can also reduce the amount of oxygen that reaches your eyes.
Other potential risk factors include obesity, certain medications, and poor diet, although the research on linking these factors to AMD is still inconclusive.
Signs of macular degeneration to watch out for
There are a few symptoms to note if you suspect you may have macular degeneration. Here are some typical examples of the common signs of macular degeneration to look out for:
- Your vision is gradually becoming more blurry
- Your eyes have difficulty adjusting to different levels of light
- You may have issues with color, depth, and texture perception
- Your vision becomes spotty
If any of these signs of macular degeneration feel familiar, check out our article on how to self-test for macular degeneration using the macular degeneration amsler grid.
Early detection is key to the successful treatment of macular degeneration. If macular degeneration is not detected soon enough, your vision can become more wavy and distorted at a quicker rate.
Can you reverse macular degeneration?
There currently are no macular degeneration treatment options that will cure you of AMD. However, if you catch the early signs, you may be able to slow the disease down. The best way to practice macular degeneration prevention is to make permanent lifestyle changes to slow the disease:
- Schedule regular eye exams
- Quit smoking
- Incorporate vitamins A, E, and C
- Improve your diet and exercise
- Protect your eyes from sunlight exposure
For a deeper understanding of AMD prevention, read our article: Macular Degeneration Prevention Tips. Treatment options for AMD include laser procedures, eye injections, and certain vitamins. For more information, speak with an ophthalmologist at Eye Center of Texas.
Don’t wait. Speak with a macular degeneration specialist at Eye Center of Texas today
Think you may be showing signs of macular degeneration? Have additional questions regarding what causes macular degeneration? A retina specialist in Houston from Eye Center of Texas can help answer your questions and work with you on how to maintain your vision. Our experience detecting and treating macular degeneration allows us to promptly answer your questions and take preventative measures.
Call 713-797-1010 or request an appointment online today.
More Helpful Articles by Eye Center of Texas:
Related Articles
Medically Reviewed by:
Wet vs. Dry Macular Degeneration
The main difference between wet vs dry macular degeneration is simple: dry macular degeneration is the more common type of eye disease and does less damage to your vision while wet macular degeneration can result in serious vision loss.
Clinically, however, there are more specific differences between wet vs. dry macular degeneration that are slightly more involved. We’ll discuss these here along with other important information about the difference between wet and dry AMD.
For more resources regarding macular degeneration, check out our articles: What is Macular Degeneration?, Common signs of macular degeneration, and 5 Macular Degeneration Prevention Tips.
What causes macular degeneration?
Before we get into the details of wet vs. dry macular degeneration, it’s important to understand what macular degeneration is, in general. Macular degeneration is a chronic eye disease that gradually destroys central vision. When the process of transporting nutrients and waste by a layer of cells called the retinal pigment epithelium (RPE) is slowed down, yellowish deposits called drusen will form underneath the retina.
An excess of drusen is a telling sign that a person may have macular degeneration. Drusen cut off oxygen to your eye and may contribute to a thinning of the macula, the part of your retina that is responsible for giving you a clear line of sight. It’s this thinning of the macula that causes the damaged or lost vision characteristic of macular degeneration.
While macular generation is associated with aging, the cause of its onset is still unknown. Research indicates other additional hereditary and environmental factors risk factors including:
- Family history
- Cardiovascular disease and high blood pressure may place additional stress on the blood vessels, accelerating the development of vision loss
- Smoking will triple the risk of developing macular degeneration
- Elevated serum lipids (cholesterol and triglycerides) have been associated with an increased risk of macular degeneration
- Complement factor H is a marker of inflammation, and abnormalities in this gene have been linked to macular degeneration
- Excessive exposure to sunlight is a risk factor for eye disease, be sure to wear sunglasses or hats to protect your eyes from harmful rays
- And more
Research has shown that proper diet, exercise, and maintaining your overall health can lower your risk of developing macular degeneration. However, age still plays a role, as the odds of developing this disease are even greater once you reach 75 years of age.
What is dry macular degeneration?
Macular degeneration can often develop in two forms: dry (atrophic) or wet (exudative). The difference between wet vs dry macular degeneration is in the severity. Dry macular degeneration is the most common type of macular degeneration and is not as serious. About 85-90% of patients who develop macular degeneration develop the dry form. Most will experience minimal vision loss and excess development of large, soft drusen in the retina. The dry form can worsen over time if not seen by a specialist, and can result in the loss of central vision.
Can dry macular degeneration be treated?
There are currently no treatments that cure dry macular degeneration. However, clinical trials are currently being done for potential treatments. Dry macular degeneration treatment breakthroughs include stem cell therapies, an injection of the drug Apl-2, an oral antibiotic called Oracea, and an anti-inflammatory drug called Metformin. Most of these potential treatments are in phases two or three of their research and may not be available until for several more years.
What is wet macular degeneration?
Wet macular degeneration is the less common yet more serious type to develop. In the wet stage of macular degeneration, new blood vessels begin to form underneath the retina (choroidal neovascularization). Unfortunately, these new blood vessels often lead to blood or fluid leakage in the retina where vision can become distorted. In this stage, consulting a doctor is crucial. A good tool for identifying any changes in your vision is the macular degeneration amsler grid, a self-administered test in which straight lines will appear distorted if there is fluid underneath your retina.
Can wet macular degeneration be treated?
Similar to the dry form, treatment for wet macular degeneration has not been established yet. The best way to treat wet macular degeneration is to prevent the disease before it happens. This can be done with injections, laser procedures, and maintaining a healthy lifestyle. If caught late, these treatment options will help manage the side effects of wet macular degeneration.
Additional wet vs. dry macular degeneration FAQs
Which is worse, dry or wet macular degeneration?
Wet macular degeneration is more serious and is the leading cause of permanent central vision loss. Though the dry type is less serious, it can lead to the wet type if not monitored closely by a doctor.
How often does dry macular degeneration turn into wet?
About 1-in-10 people who suffer from dry macular degeneration will eventually develop wet macular degeneration. Though not as common, it’s still possible, so be sure to visit your eye doctor regularly if you already have dry macular degeneration.
How can I avoid macular degeneration?
Even if you aren’t experiencing any symptoms of macular degeneration, early prevention is your best chance at stopping or slowing down the disease. Luckily, the prevention tips are easy to follow — see your eye doctor regularly, prioritize diet and exercise, don’t smoke, take vitamins, or consider other types of prevention therapy as recommended by your doctor.
Spot the signs early, save your eyesight: Contact Eye Center of Texas today.
If you are over the age of 50 and notice some of the signs and symptoms of macular degeneration like worsening eyesight, blurred vision, etc. we recommend you visit our retina specialist here at Eye Center of Texas.
We are here to help answer any questions you may have regarding wet vs. dry macular degeneration, eye health tips, and more.
Spotting macular degeneration early can help to avoid vision loss in the future. Give us a call at 713-797-1010 or request an appointment online today.
More Helpful Articles by Eye Center of Texas:
Related Articles
Medically Reviewed by:
5 Macular Degeneration Prevention Tips
Why concern yourself with macular degeneration prevention if you don’t have the condition? While it is possible to stop or slow the progression of age-related macular degeneration once you’ve been diagnosed, there is currently no cure if you’re diagnosed with AMD.
In other words, once you have AMD, you’ll want to make permanent changes to your lifestyle habits to slow down the progression of the disease. If you don’t, then you may eventually suffer drastic loss of vision.
Luckily for those concerned about macular degeneration, prevention tips are simple to follow. A little education on macular degeneration causes and prevention can go a long way. Let’s break down a few easy-to-follow macular degeneration prevention tips now.
Need a review of the causes, signs, symptoms, and treatments of macular degeneration? Check out our article: What is Macular Degeneration?
Tip #1: Don’t skip your eye exams
At the top of our list of macular degeneration prevention tips is making sure that you schedule and go to regular eye exams. While eye exams won’t exactly prevent macular degeneration, they can give you the opportunity to catch the diseases early and prevent the disease from progressing. During an eye exam, your doctor will look for the initial signs of macular degeneration. If spotted, you can immediately begin AMD treatment recommendations and as a result, slow down its progression.
The frequency of regular eye exams should increase as you age, with those over the age of 50 attending an eye exam at least once every one to two years.
Think you might be showing signs of macular degeneration? Check out our article on how to self-test using the Amsler grid screening test.
Tip #2: Take your vitamins
Whether or not you’ve been diagnosed with AMD, some vitamins may help delay the onset or s progression of the disease. But if you’re wondering, “What vitamin can you take to help prevent macular degeneration?” — that’s not exactly how this tip works.
According to studies, including this Harvard macular degeneration study, a simple (yet high-dosed) vitamin cocktail that includes vitamins such as vitamins A, E, and C can slow the progression of macular degeneration. However, taking a consistently high dosage of these vitamins has not been shown to prevent the disease from setting in altogether. Many doctors would even recommend a better diet over a surplus of vitamins (prior to a diagnosis).
Tip #3: Quit smoking
Smoking can negatively impact your body in more than ways, but many people don’t realize that smoking can impact your vision, as well. In fact, smoking is considered one of the leading causes of macular degeneration and a major contributing factor of its progression; Research shows that smokers are 2 to 5 times more likely to succumb to macular degeneration than non-smokers are. In other words, if you want to prevent or slow down AMD, then make this macular degeneration prevention tip one of your top priorities.
Tip #4: Improve your diet and exercise
Similar to smoking, those with a poor diet and lack of an exercise routine are more susceptible to macular degeneration. A poor diet can lead to issues with your blood sugar, blood pressure, and cholesterol — all of which can negatively impact eye health. Couple these issues with little-to-no exercise and you’re considered to be 2 to 3 times more likely to suffer from AMD. Long story short, if you include more greens and walking in your life, macular degeneration will be less likely to pop up.
The American Macular Degeneration Foundation (AMDF) has created a guide to eating right for your eye health, including information on macular degeneration foods to avoid. Eye Center of Texas has also published a guide to the best foods for eye health (originally geared toward diabetics, but applicable to all patients).
Tip #5: Consider drug therapy
As a treatment option for wet macular degeneration, Vascular Endothelial Growth Factor (VEGF) inhibitors have been shown to significantly help prevent the progression of AMD. In some cases, VEGF inhibitors have even helped those suffering from wet AMD recover some of their lost vision. These particular drugs are used to reduce swelling, as well as the formation of new blood vessels (both of which are issues that can negatively impact your macula and lead to further vision loss).
VEGF inhibitors have shown to cause other health issues, so it’s important to speak with your doctor and weigh all your options before beginning this macular degeneration treatment option.
Want more help than macular degeneration prevention tips? Contact Eye Center of Texas.
These 5 macular degeneration prevention tips can help prevent and slow down AMD’s progression. However, comprehensive treatment of macular degeneration requires routine appointments with your eye doctor and consistent improvements with your lifestyle choices and habits.
AMD is a common eye disease that many people struggle with on a daily basis. If your eyesight is getting worse, if you’re over the age of 50, or if eye disease runs in the family, the time to take preventative action is now.
At Eye Center of Texas, you can speak with a leading retina specialist in Houston and get expert help maintaining your eye vision for as long as possible. We are here to answer your macular degeneration questions, from, “What is the best treatment for macular degeneration?” to clarification regarding dry vs. wet macular degeneration.
Call us at 713-797-1010 or fill out our online form to request an appointment today.
More Helpful Articles by Eye Center of Texas:
Related Articles
Medically Reviewed by:
The Most Common Signs of Macular Degeneration
Since there is currently no cure for the disease, catching the signs of macular degeneration can be critical for the future of your vision. If you watch for the early signs of macular degeneration, it might be possible to slow down the progression of this particular eye disease.
Your susceptibility to this disease grows as you age, and it is becoming increasingly common for those over the age of 70 to be diagnosed with some degree of macular degeneration. In fact, as far as common vision problems go, macular degeneration is one of the leading causes of vision loss in older adults.
Before we cover the early signs of macular degeneration, we will quickly review the various causes and types of this eye disease. We also cover this information more in-depth in our article, What is Macular Degeneration? If you are already familiar with this information, simply skip directly to the early signs of macular degeneration.
What is the main cause of macular degeneration?
The exact cause of macular degeneration is unknown. However, as mentioned previously, your susceptibility to macular degeneration increases as you age, so in some sense, aging is considered a main cause of the disease.
There are other factors that can make you even more susceptible. These factors can include:
- Lifestyle habits such as smoking and lack of exercise
- Gender, as women may be more at risk
- Family genes.
If you fall under any of these categories, then you will want to monitor for the signs of macular degeneration regularly.
The cause of the physical symptoms of macular degeneration is the wearing down of the central part of your retina. The retina is made of tissue at the back of your eye and is composed of light-sensitive cells (called rods and cones). When these become worn down you begin to experience vision loss, especially central vision loss.
What are the different types of macular degeneration?
There are two types of macular degeneration: dry macular generation (non-neovascular) and wet macular degeneration (neovascular).
What you should know about dry macular degeneration:
- The most common type of macular degeneration
- Not as serious as wet macular degeneration
- Minimal vision loss typically experienced
- Development of drusen (small yellow or white spots on the retina) upon accumulation of waste products
What you should know about wet macular degeneration:
- The more serious (albeit the less common) type of macular degeneration
- Leads to the formation of new blood vessels causing fluids or blood to leak into the retina
- Vision might appear wavy or distorted
FAQ: Are floaters a symptom of macular degeneration?
Typically, no. The spots in your vision created by macular degeneration can be confused with floaters but, with the exception of late-stage wet macular degeneration, macular degeneration itself rarely causes floaters.
What are the common signs of macular degeneration?
With macular degeneration, your vision will generally gradually become less clear and more blurry. Day-to-day life and activities like driving, using your smartphone, reading, and even recognizing people may feel difficult or problematic. Here, we break down the common signs of macular degeneration a little further.
Difficulty adapting to changing light
If you have trouble with lighting changes, this may be a sign of macular degeneration. With this particular sign, you may have issues with levels of light suddenly changing. For example, if you go from a dark room to a light room (or vice versa), your eyes might struggle to adapt. You may also have issues performing simple tasks without a high level of light present.
Issues with depth, color, and texture perception
This particular sign of macular degeneration can affect you in a variety of ways — all of which can be somewhat dangerous given the situation. In this case, you may have trouble judging how close or far away something is. You may also have trouble judging similar colors or textures. In both cases, you can be more susceptible to falling or tripping.
Spotted vision
Macular degeneration can also come with dark spotting in your line of vision. This might present itself as just a blurry spot or it could be a dark or shadow-like blurry spot.
Overall blurring
While you may have a blurry spot in your line of vision, you could just have altogether blurrier vision. This could mean difficulty trying to recognize faces, reading books or labels, or using digital devices.
Macular degeneration treatment
Once macular degeneration sets in, you can’t get rid of it; there is no cure. So if you’re over the age of 50 and notice that your eyesight is getting worse or other signs of macular degeneration, we encourage you to schedule an appointment with a retina specialist in Houston. Spot it early, and you can avoid additional vision loss.
Macular degeneration treatments for helping you to reduce further damage and, in the case of wet macular degeneration, manage side effects.
Treatment options for dry macular degeneration:
- Nutritional supplements
- Sunglasses (eye protection)
- Healthy lifestyle choices
- Monitoring blood pressure and cholesterol
Treatment options for wet macular degeneration:
- Injections directly into the eye
- Laser procedures
- Healthy lifestyle choices
Many of these treatments boil down to simply doing right by your body. Keep in mind, however, that many of these treatments can help prevent macular degeneration as well.
Detect signs of macular degeneration early at Eye Center of Texas
Eye Center of Texas is home to some of the most skilled Houston ophthalmologists. We have experience detecting and treating macular degeneration, and we help hundreds of Texans protect and correct their vision every year.
If you think you’re experiencing signs of macular degeneration or if you’d like more information on this common eye disease, schedule an appointment today or give us a call at 713-797-1010.
More Helpful Articles by Eye Center of Texas
Related Articles
Medically Reviewed by:
Living with AMD
While there is no cure for Age-related Macular Degeneration (AMD), there are steps you can take to help reduce your risk of progression.
Monitor your vision weekly.
Use an Amsler grid, a tool that helps you monitor subtle changes in your central vision. Some forms of AMD can progress very quickly. Monitoring your vision weekly can help you notice any changes. If you do notice changes, talk to your eye doctor immediately.
Keep your eye doctor appointments.
Experts recommend a comprehensive eye exam at least once a year for everyone. Some changes in vision may be best detected by an eye care professional, so it’s important to keep your eye appointments, as directed.
If you smoke, quit.
We know it’s not easy. But stopping smoking may be the most important thing you can do to help reduce your risk of AMD progression. Consider creating a plan to stop smoking that is tailored specifically to your needs and habit.
Maintain your overall health. High cholesterol and blood pressure can increase your risk of AMD. Try to exercise for 30 minutes a few times a week. Consult your doctor before starting any exercise routine. Strive for a balanced diet rich in fruits and vegetables, particularly dark, leafy greens. Get your blood pressure and cholesterol levels checked.
Consider low-vision aids.
Many people with AMD may also benefit from the help of low-vision aids, devices designed to help people with low vision function better, such as handheld magnifiers.
Related Articles
Medically Reviewed by:
National AMD and Low Vision Awareness Month
February is National Age-related macular degeneration (AMD) /Low Vision Awareness Month. Age-related macular degeneration is the leading cause of vision loss for individuals age 50 and older. Macular degeneration is a progressive, usually painless disease that affects the macula, the spot on the retina at the back of the eye responsible for central vision, causing central vision to blur, but leaving peripheral vision intact. In its earliest stages, AMD can be difficult to diagnose. In some cases, AMD progresses so slowly that many do not notice a change in their vision. In other cases, the deterioration is very rapid and can appear to happen overnight.
There are two major types of AMD, a “dry” and a “wet” form. The dry form is the early stage and is the most common form of AMD. There is usually little or no vision loss during this stage although there are exceptions with some people having significant vision loss from more advanced “dry” degeneration. The wet form is a late stage of the condition and affects about 10 percent of all people with the condition. Wet AMD accounts for the majority of central vision loss due to AMD.
The wet stage is when abnormal blood vessels start to grow beneath the center of the macula and, as they grow, they leak fluid or blood and cause central vision loss with blurring and distortion of vision. Untreated, these abnormal blood vessels typically will grow relatively large and eventually cause scarring with permanent and often severe central vision loss.
Signs & Symptoms of AMD (If you notice changes to your vision in the following areas you should speak with your doctor particularly if you are older than 50):
- You notice a blurred / blind spot in the center of your field of vision
- You require more light when reading
- You find it difficult to adapt to low lit areas
- Printed words become slightly blurry
- Colors do not seem as bright
- Sometimes you have difficulty recognizing faces
- Your overall vision is becoming hazy
Causes of Macular Degeneration
Even though there is no known exact cause for Macular Degeneration, its origins are considered multi-factorial and the following factors may place you at a higher risk:
- Family history of Macular Degeneration
- Low macular pigment density
- Smoking
- High cholesterol
- Farsightedness
- Poor Diet / Obesity
- Sun exposure
What is Low Vision?
People with low vision find everyday tasks difficult to do – even with the aid of regular glasses, contact lenses, medicine or surgery. Reading the mail, shopping, cooking, seeing the TV and writing can seem challenging.
Just one more reason to see your eye doctor regularly for early detection of AMD. To schedule an appointment, call our office at 713-797-1010 or schedule an appointment using our convenient online form
Related Articles
Medically Reviewed by:
Reduce Your Risk for AMD & Heart Disease
February is National Heart Disease Awareness Month and Age-Related Macular Degeneration (AMD) and Low Vision Awareness Month.
Some of the same things that put you at risk for heart disease and stroke also put you at risk for AMD. These include:
- High blood pressure
- High cholesterol
- Obesity
- Smoking
The good news is that you can lower your blood pressure and cholesterol to reduce your risk of heart disease and AMD by:
- Consult a doctor; follow their instructions and stay on your medications.
- Eat a healthy diet that is low in salt; low in total fat, saturated fat, and cholesterol; and full of fresh fruits and vegetables.
- Take a brisk 10-minute walk, 3 times a day, 5 days a week.
- Don’t smoke and if you do smoke…quit!!!
Related Articles
Financing Options Available
Apply today to find a financing option that meets your needs.
Our Locations
Houston/Bellaire
6565 W. Loop S., Suite 650Bellaire, TX 77401
Medical Office:
713-797-1010
Medical Fax:
713-357-7276
LASIK/Near Vision:
Office: 713-395-1515
Fax: 713-357-7278
Pasadena
4415 Crenshaw RoadPasadena, TX 77504
Medical Office:
281-977-8800
Medical Fax:
281-977-8877
Sugar Land
15200 S.W. Freeway, Suite 130Sugar Land, TX 77478
Medical Office:
281-277-1010
Medical Fax:
281-277-4504
Clear Lake
455 E. Medical Center Blvd., Suite 110Webster, TX 77598
Medical Office:
281-332-1397
Medical Fax:
281-282-9152
Katy
Greenhouse Medical Plaza2051 Greenhouse Road, Suite 110
Houston, TX 77084
Medical Office:
346-547-7070
Medical Fax:
281-214-2971
The Woodlands/Conroe
100 Medical Center Blvd., Suite 118Conroe, TX 77304
Medical Office:
936-647-1610
Medical Fax:
936-647-1620