Macular Degeneration Specialist in Houston
If you or a loved one is suffering from macular degeneration, you need to contact a macular degeneration specialist in Houston to talk about prevention, diagnosis, and treatment. Macular degeneration is the most common cause of severe vision loss in people over the age of 50, with more than 8 million people in the U.S. alone having some form of this disease.
Wondering how macular degeneration is diagnosed? The differences between wet vs dry macular degeneration? How macular degeneration can be treated and prevented? You’ll find your answers here.
It’s important to spot the signs of macular degeneration early if you want to minimize damage to your eyesight. Call Eye Center of Texas at (713) 797-1010 or make an appointment online to see a specialist today!
Age-related macular degeneration
While the term “macular degeneration” includes many different eye diseases, all of them cause degeneration of the most central and sharpest vision. Age-related macular degeneration is the most common of these disorders, mainly affecting people over the age of 60.
Age-related macular degeneration (AMD) is an eye disease that primarily affects the central portion of the retina known as the macula. The risk of developing macular degeneration increases with age and is in excess of 30% by age 75. Other risk factors include a family history of the disease, cigarette smoking, poor diet, excessive sunlight exposure, hypertension, and cardiovascular disease.
AMD is classified as either wet macular degeneration (neovascular) or dry macular degeneration (non-neovascular). About 10% of patients who suffer from macular degeneration have wet AMD.
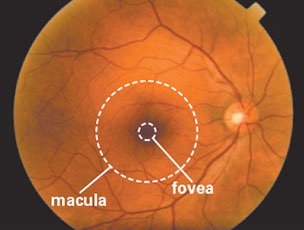
This photograph shows a normal, healthy retina as viewed by an eye doctor during an examination. The ophthalmologist will pay careful attention to the appearance of the macula and fovea to formulate a diagnosis.
Dry macular degeneration
The majority of people with macular degeneration have an early form of the condition and experience minimal vision loss. For many of these people, macular degeneration will not progress to a more serious condition. How does macular degeneration work?
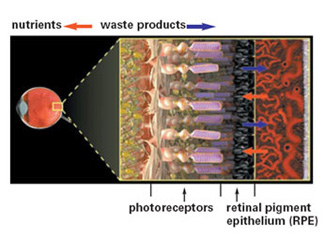
In the early stages of macular degeneration, the transport of nutrients and wastes by the retinal pigment epithelium (RPE) slows down. As waste products accumulate under the retina, they form yellowish deposits called drusen.
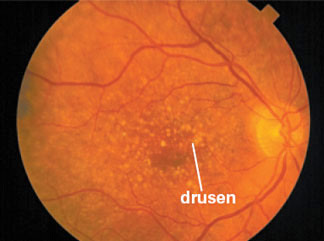
An eye doctor examining a patient at this stage may note the presence of these drusen, even though most people have no symptoms. Once drusen have been noted, monitoring will be needed over time, although most patients will not progress to develop vision loss. Many people over the age of 60 will have some drusen.
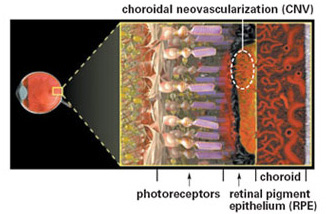
In the healthy retina, the RPE supplies the photoreceptors with nutrients and pumps out the waste products created as the photoreceptors convert light into nerve signals.
A portion of people with drusen may begin to experience mild vision loss. At this point, macular degeneration may progress in one of two ways. These two types of degeneration are known as dry macular degeneration (atrophic) and wet macular degeneration (exudative).
This retinal photograph shows numerous yellow drusen in and around the macular region of the retina.
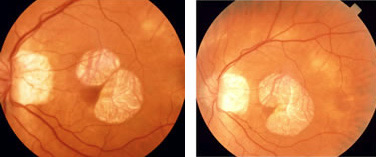
Eyes with geographic atrophy, a variant of dry macular degeneration, develop a wearing away of the macular pigmented tissues. The atrophy causes discrete islands of blind spots. Vision is good unless the atrophy extends into the macular center.
While geographic atrophy spares the macular center, the atrophy will gradually enlarge and cause loss of vision.
Wet macular degeneration
For reasons that are not fully understood, a minority of people with macular degeneration develop a more serious form of the disease. People with large “soft” drusen (drusen with indistinct borders), many drusen that run together, or focal pigmentation are at greater risk for developing the wet (exudative) form of the disease.
In wet macular degeneration, new blood vessels grow underneath the retina in a process called choroidal neovascularization (CNV).
It is believed that the diseased retina stimulates the production of these new blood vessels in response to a decreased supply of nutrients and slow transport of wastes. Unfortunately, new blood vessels do not improve the health of the retina. Instead, they often leak blood or fluid into the retina.
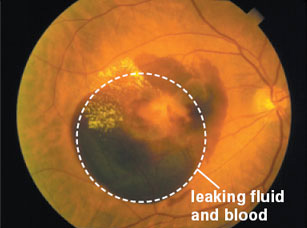
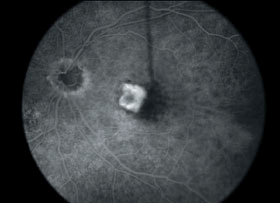
This retinal photograph shows fluid and blood beneath the retina, which suggests the presence of choroidal neovascularization (CNV).
As CNV continues, blood or fluid may leak under the retina, causing the retinal surface to become uneven, and making objects in that portion of your visual field appear wavy or distorted. Blind spots may appear in your vision if portions of the retina become damaged by the CNV.
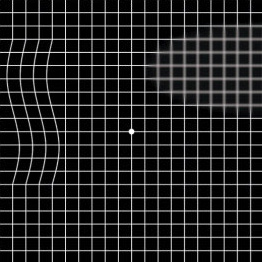
Often the first sign of fluid under the retina is a distortion of straight lines. Since these changes can be subtle, regular testing with the Amsler grid, shown here, can be helpful in the early detection of problems.
Any change in the appearance of the macular grid may be a sign of choroidal neovascularization and should prompt a visit to the eye doctor. If caught early enough, the CNV might be treatable before it causes too much damage. If CNV is allowed to progress unchecked, it can lead to the death of the overlying photoreceptors and scarring of the macula, and result in significant vision loss.
Should you see a specialist for macular degeneration?
Who is the best doctor to treat macular degeneration? A retina specialist, or retinologist, would have the most experience in the examination and diagnosis of macular degeneration.
A thorough examination by a retina specialist is the best way to determine if you exhibit any of the common signs of macular degeneration, and either have macular degeneration or are at risk of developing the condition.
The exam begins by testing your visual acuity and then testing for areas of distorted or reduced vision, both common symptoms of macular degeneration. If you do have macular degeneration, your doctor will use the Amsler grid to determine if your vision has changed.
After these visual tests, the front part of your eyes will be examined to determine if everything is healthy. Your doctor may put anesthetic drops in your eyes before measuring the pressure in each eye. Drops are administered to dilate your pupils, after which the eye doctor will seat the patient at a device called a slit lamp.
Under the slit lamp, your doctor will look for drusen and other areas of the retina that might appear suspicious or abnormal. After which further examination is needed to confirm the presence of choroidal neovascularization (CNV). Here are some examples of examinations a specialist may perform.
Angiography
Angiography is the most useful test for determining the presence of choroidal neovascularization (CNV). The procedure is painless and very safe. During the process, the patient is seated at a fundus camera, which takes pictures of the retina, and a small IV catheter is inserted into a large vein.
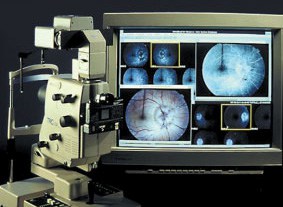
The fundus camera takes pictures of the fundus or retina, while the catheter is inserted to inject fluorescein or ICG dye. As the dye enters the blood vessels of the eye, a series of photographs are taken of the retina. By looking at the pattern of the blood vessels and observing whether dye leaks from any of the vessels as time passes, your ophthalmologist can locate sites of choroidal neovascularization if they are present.
This fluorescein angiogram shows choroidal neovascularization (CNV) in the macula. The bright area indicates dye leaking from the neovascular vessels.
Optical Coherence Tomography
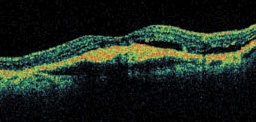
Optical Coherence Tomography (OCT) is a new technique for imaging the retina. It is a non–invasive test that records the features of the retina and displays this information as cross-sectional views or optical “slices.”
Laser light is used to map the anatomy of the retina, and the resulting computer images are saved for analysis. OCT evaluations are not a replacement for angiography, rather they are complementary techniques.
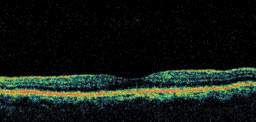
Note the differences between the two images. The top image is a normal eye, representing smooth, even layers of the retina, while the bottom image is an eye with wet macular degeneration, containing retinal layers that are no longer smooth and flat.
Macular degeneration treatment and research
What is the newest treatment for macular degeneration? There is a wide range of treatments available for macular degeneration, ranging from drug therapy and laser surgery, all the way to newer, more experimental therapies. Some of the more popular options include:
- Pharmacologic therapy treatments including Macugen, Lucentis, Avastin, and Visudyne Photodynamic Therapy
- Laser treatment
- Rheopheresis
- Low-dose radiation therapy
- Submacular surgery
- RPE transplant
- Macular translocation surgery
- Artificial vision
Although there are many effective treatments for macular degeneration, there is no cure for the chronic disease process. For this reason and for the hope of better visual results for the patient, many new methods of treatment are being developed and tested.
It is important to note that other than laser treatment and pharmacologic treatment, all of the methods mentioned above are still considered somewhat experimental.
Learn more about the latest treatment for dry macular
Macular degeneration risk factors
A number of factors are known to increase the risk of developing macular degeneration. Some of these factors are within an individual’s control and can be modified through changes in behavior.
The following factors may increase your risk of developing age-related macular degeneration:
- Age
- Family history of the disease
- Smoking
- High blood pressure
- History of cardiovascular disease
- Elevated serum lipids
- Complement factor H
- Excessive exposure to bright sunlight
The rate of macular degeneration in the population clearly increases with age. By age 75, the odds of having this condition are greater than 1 in 3. If your parent or sibling has macular degeneration, you have an increased risk of developing the disease yourself. If any of these factors apply to you and you are wondering when to see an ophthalmologist, the time might be now.
Macular degeneration prevention
Studies have shown that the role of nutrition is paramount in the development of macular degeneration. An important research study, the Age-Related Eye Disease Study (AREDS), showed that one group of patients at high risk for developing advanced AMD lowered their risk by about 25 percent when treated with high doses of both zinc and antioxidants.
Research has also shown that patients who eat diets high in spinach or collard greens are less likely to develop macular degeneration. These and other green leafy vegetables are good sources of two important macular pigments: lutein and zeaxanthin. Also recommended for macular health are diets high in omega-3 fatty acids and zinc.
Need a macular degeneration specialist in Houston? Eye Center of Texas can help!
A macular degeneration specialist in Houston from Eye Center of Texas can help you catch signs of macular degeneration early and help save your vision. Our specialists have the training and cutting-edge technology to detect and diagnose your macular degeneration, as well as recommend a treatment path that can help you protect your vision.
If you or a loved one is experiencing vision loss or distortion and believe it to be macular degeneration, give Eye Center of Texas a call at (713) 797-1010 or make an appointment online today!
Financing Options Available
Apply today to find a financing option that meets your needs.
Our Locations
Houston/Bellaire
6565 W. Loop S., Suite 650Bellaire, TX 77401
Medical Office:
713-797-1010
Medical Fax:
713-357-7276
LASIK/Near Vision:
Office: 713-395-1515
Fax: 713-357-7278
Pasadena
4415 Crenshaw RoadPasadena, TX 77504
Medical Office:
281-977-8800
Medical Fax:
281-977-8877
Sugar Land
15200 S.W. Freeway, Suite 130Sugar Land, TX 77478
Medical Office:
281-277-1010
Medical Fax:
281-277-4504
Clear Lake
455 E. Medical Center Blvd., Suite 110Webster, TX 77598
Medical Office:
281-332-1397
Medical Fax:
281-282-9152
Katy
Greenhouse Medical Plaza2051 Greenhouse Road, Suite 110
Houston, TX 77084
Medical Office:
346-547-7070
Medical Fax:
281-214-2971
The Woodlands/Conroe
100 Medical Center Blvd., Suite 118Conroe, TX 77304
Medical Office:
936-647-1610
Medical Fax:
936-647-1620